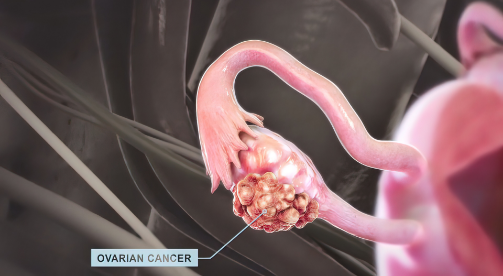
Cancer of the ovaries is referred to as ovarian cancer. A female's ovaries are a pair of organs responsible for producing eggs and hormones.
The lifetime risk of any woman developing ovarian cancer is less than 2 %, with peak incidence at the ages of 55 and 60. However, it can also affect women who are younger than 20 years of age. In most cases, ovarian cancer arises from the surface of the ovary (epithelial cancer), and a small percentage arises from the egg cells (germ cell cancer). Cancers of the ovaries are difficult to detect early because it tends to have no or minimal non-specific symptoms, (compared to cancers of the cervix (cervical) and endometrium (lining of the uterus). As a result, screening for ovarian cancer is difficult.
Few carcinogenic agents like asbestos in talcum powder have been implicated, but they are largely unknown. Lately, research has pointed to possible certain virus infections but still unclear.
In a smaller percentage of cases, genetic susceptibility due to mutation has been shown to be responsible for causing ovarian and breast cancers.
The most important is the BRCA mutation.
Apart from BRCA mutation, which has strong risks towards the development of ovarian cancer, the specific situation is known to be associated with higher risks of ovarian cancer development. These include being
On the other hand, pregnancy, breastfeeding and contraceptive pills have been shown to reduce risks.
It is common for ovarian cancer to present with no specific symptoms or no symptoms at all in its early stages.
Bloating may be experienced by some women, while others may experience diarrhoea or constipation.
Often, these conditions are attributed to common intestinal problems and are not given the attention they deserve. Abdominal swelling tends to be mistaken for over-eating or putting on weight.
Pain only occurs when the ovarian mass is twisted on its blood supply or undergoes bleeding or rupture, which are not common.
When gross ascites (fluid) in the peritoneal cavity causing distension, it tends to present with loss of appetite and loss of weight as well. These, however, are signs of advanced cancer with spread to adjacent structures.
Detection of ovarian cancer can be divided into two broad categories. First is the screening / possible detection of very early-stage ovarian cancer, and second, the detection or diagnosis of ovarian cancer at a relatively early stage.
Extensive studies have been conducted to identify early-stage ovarian cancer, mainly using ultrasound (Transvaginal or abdominal scan) coupled with tumour markers, especially CA 125. None so far has been shown to be effective in screening. This is because there is no recognisable pre-cancerous stage in ovarian cancer comparable to cervical or even endometrial cancer.
Other tumour markers like AFP, CEA and beta HCG are not useful in screening but are only used after a mass has been diagnosed to determine the possible type of ovarian cancer and as baseline pre-surgery reference.
The only exception is screening for BRCA mutation.
Those women screened positive for this mutation has a 40-50% chance of developing ovarian and breast cancers at an earlier age. Prophylactic removal of the ovaries and, occasionally, the breasts helps to reduce the risks.
The second category is early detection or diagnosis of already developed ovarian cancer. Due to its silent nature, most cases present late in advanced stage 3C, where surgery tends to be aggressive, more complicated and has higher morbidity with higher risks of recurrent.
It is more important in younger women who have yet to start or complete their family. Earlier detection allows a diagnosis to be made at stage 1 or 2 when surgery is easier, and fertility-sparing surgery may still be possible.
This can easily be achieved as co-testing, during routine cervical cancer screening, as an opportunity to assess the risks for other female cancers.
Ovaries are intraperitoneal organs, and when they become cancerous, the main spread is within the peritoneal cavity, especially to adjacent pelvic structures like the bowel, bladder, the appendix and later to the upper abdomen like the omentum. It can also spread via the lymphatic system to local and distant lymph nodes and via blood to bone, liver and lungs.
Depending on the presentation stage, your gynaecologist will:
During the second consultation, the blood results, the tumour markers, and the CT scan findings will be discussed to determine a decision for surgery or the use of pre-surgery chemotherapy.
Expect your doctor to fully explain the planned procedure or the various stages of your cancer management. You need to ask about any uncertainty or clear your worries with the doctor. Get a second opinion on your management if you need to.
It is advisable to bring along your spouse or another companion during the consultation.
Surgery is almost certain in any ovarian cancer management to remove and stage the disease. The radicality depends on the stage and wishes for reproductive preservation.
The minimum for fertility-sparing will involve the removal of the affected ovary, omentum and related lymph nodes. In most advanced cases, surgery usually involves completely removing the uterus and ovaries, the omentum, the appendix, and any enlarged nodes or suspicious mass.
With the exception of early-stage cancer, most ovarian cancer cases will need adjuvant chemotherapy post-surgery. The most commonly used agents are platinum-based, like Carboplatinum and Taxol. The agents used for germ cell cancer in younger women include platinum, Etoposide and bleomycin. Targeted therapy and anti-vascular formation are newer agents in use when indicated.
Radiotherapy is not usually part of the treatment modality except in special circumstances.
Your gynaecologist or clinical Oncologist may order post completion CT scan with tumour markers. The follow-up schedule is usually every three to four months with tumour markers, clinical examination and ultrasound examination for the first two years. A CT scan sometimes is performed periodically or when indicated.
It is essential to understand that the diagnosis of any cancer can be a piece of devastating news to anyone. Support from the spouse and immediate family members is very important as part of the management. The support may come from moral support and encouragement to go through the treatment. Financial support is also essential, as treatment is costly and more important if the diagnosis leads to loss of employment.
It is widely recognised that the SJMC Cancer & Radiosurgery Centre is an industry leader in cancer treatment. This facility was designed to provide patients with the highest care possible.
The centre’s staff and doctors aim to provide every patient with the highest quality of care. Whether patients seek preventive services or receive therapy, their ultimate goal is to enhance their emotional and physical well-being. Additionally, the facility offers support groups and other services that can ease the burden of living with cancer daily.